Healthcare-associated infections (HAIs) are infections associated with the treatment of patients in healthcare settings, which were not originally present on the patient’s admission.1 This means a patient acquired a new infection from their healthcare stay or treatment.
The Most Frequent Medical Adverse Event
HAIs are the most frequently occurring medical adverse event worldwide, with a prevalence of around 7-10%.2,3
HAIs are a serious patient safety issue and burden to society.4,5 Facilities and practitioners may also suffer financial as well as reputational damage as a result of HAIs associated with their facility.
HAIs Add Considerable Cost to Delivering Healthcare
HAIs are a significant cost to the Canadian healthcare system.5 Researchers have estimated 8000-12000 deaths per year are linked to HAIs, making them the fourth leading cause of death for Canadians behind cancer, heart disease and stroke. 4,5
HAIs are Preventable
A systematic review and meta-analysis found 35-55% of HAIs are preventable with existing multifaceted infection prevention and control interventions, regardless of a country’s income level.6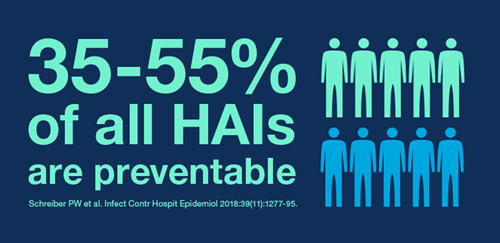
The Role of Medical Devices in HAIs
Sterilization and disinfection of medical devices play an important role in the prevention of HAIs. Multiple studies document failures in medical device reprocessing, some of which have led to outbreaks and patient exposure.7-9
In 2014 the Government of Saskatchewan's Infection Prevention and Control Program released an alert on the improper reprocessing of transvaginal ultrasound probes. The alert included a call to action for healthcare facilities to ensure all necessary reprocessing steps for reusable medical devices were being followed to meet Accreditation Canada and the Canadian Standards Association (CSA) standards for reprocessing. 10
The U.S. Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) released a Health Alert in 2015 urging healthcare facilities including hospitals, ambulatory surgical centers, clinics, and doctors’ offices, review all reusable medical device reprocessing practices.11
In 2017 the Joint Commission in the USA released a Quick Safety Alert that reported 74% of all immediate threat to life declarations (ITLs) were from improper sterilization or high level disinfection (HLD) of reusable medical devices.11 Noncompliance with TJC infection control standards had increased in hospitals, critical access hospitals, ambulatory and office-based surgery facilities.12
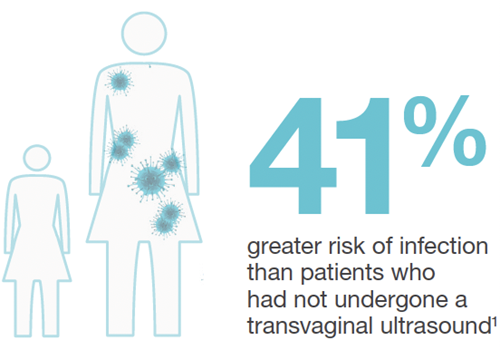
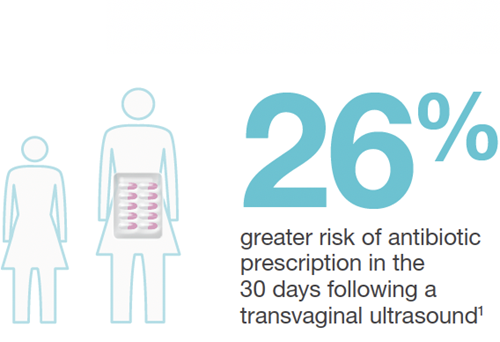
Population Level Study: Infection Risk after Ultrasound
In the first of its kind, a study commissioned by UK National Health Authorities (Scotland) revealed an "unacceptable risk" of patient infection following ultrasound. The study revealed an increased infection risk in the 30 days following endocavitary ultrasound. Commissioned by a national health authority, the study revealed an increased infection risk in the 30 days following endocavitary ultrasound.13
90.5% of facilities were not performing HLD of these probes at the time of the study.
Public Health Risk Reality
Of the 982,911 patients followed, 330,500 were gynecological patients.
60,698 of these patients had undergone transvaginal ultrasound.

The national health authority now recommends HLD for endocavitary ultrasound probes.
The increased rates of infection risk following transvaginal ultrasound were startling:13
Prevent HAIs from Medical Devices
The Spaulding Classification identifies the level of disinfection or sterilization required for medical devices based on the expected patient tissue the device will contact.
The Spaulding Classification forms the basis of international ultrasound probe reprocessing guidelines.
Internationally, Federal authorities and professional societies provide guidance on the proper reprocessing of ultrasound probes, to help keep patients safe from HAIs.
These guidelines are based on The Spaulding Classification.
Learn when to High Level Disinfect ultrasound probes
Learn about the clinical risks from improper ultrasound probe reprocessing
References
1. World Health Organization (WHO) 2020. Infection prevention and control. The burden of health care-associated infection worldwide. Webpage accessed October 2020.
2. Currie K, et al. Am J Infect Control. 2018;46(8):936-42.
3. World Health Organization (WHO). Healthcare Associate Infections Fact Sheet. Accessed online October 2020.
4.PICNet 2021 [website]. Surveillance. About Healthcare-associated Infections. Accessed July 2021.
5. Government of Canada 2021 [website]. Canadian Nosocomial Infection Surveillance Program (CNISP): Summary Report of Healthcare Associated Infection (HAI), Antimicrobial Resistance (AMR) and Antimicrobial Use (AMU) Surveillance Data from January 1, 2013 to December 31, 2017. Accessed July 2021.
6. Schreiber PW, et al. Infect Control Hosp Epidemiol. 2018;39(11):1277-95
7. WHO 2016. Decontamination and Reprocessing of Medical Devices for Health-care Facilities.
8. CDC 2008. Guideline for Disinfection and Sterilization in Healthcare Facilities.
9. Rutala WA, Weber DJ. Infect Dis Clin North Am. 2016 Sep;30(3):609-37.
10. Government of Saskatchewan Infection Prevention and Control Program. Alert: Improper Reprocessing of Transvaginal Ultrasound Probes. November 2014. Accessed online July 2021.
11. CDC & FDA 2015. Healthcare Alert Network. HAN 00382 & HAN 00383.
12. TJC 2017. Improperly sterilized or HLD equipment – a growing problem. Issue 33. May 2017.
13. Scott D et al. Ultrasound 2018;26(3): 168-177.
